Interventional Clinical Study Process Model
Jump to navigation
Jump to search
A Interventional Clinical Study Process Model is a clinical study sequence model for a clinical trial processs.
- Context:
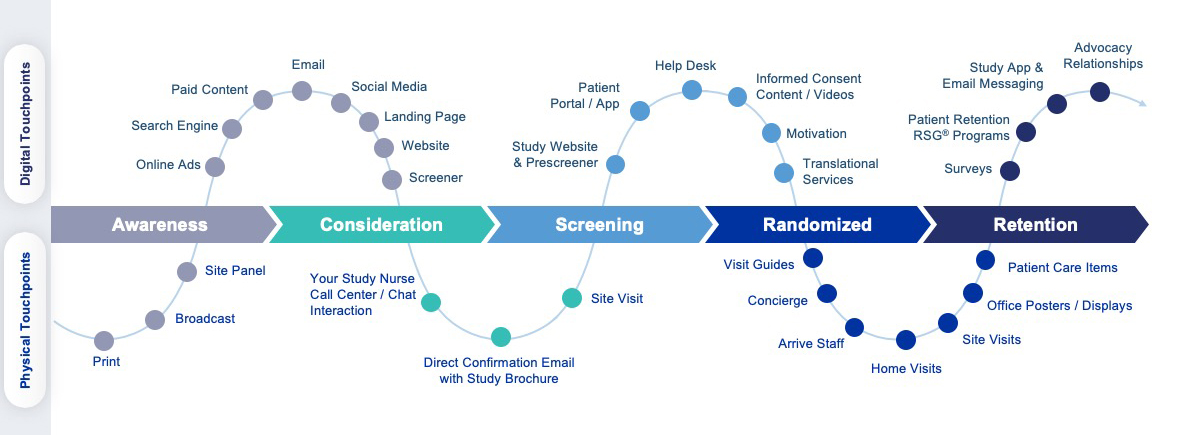
- It can include a Clinical Trial Sponsor Representation Model or a Clinical Trial Patient Journey Model.
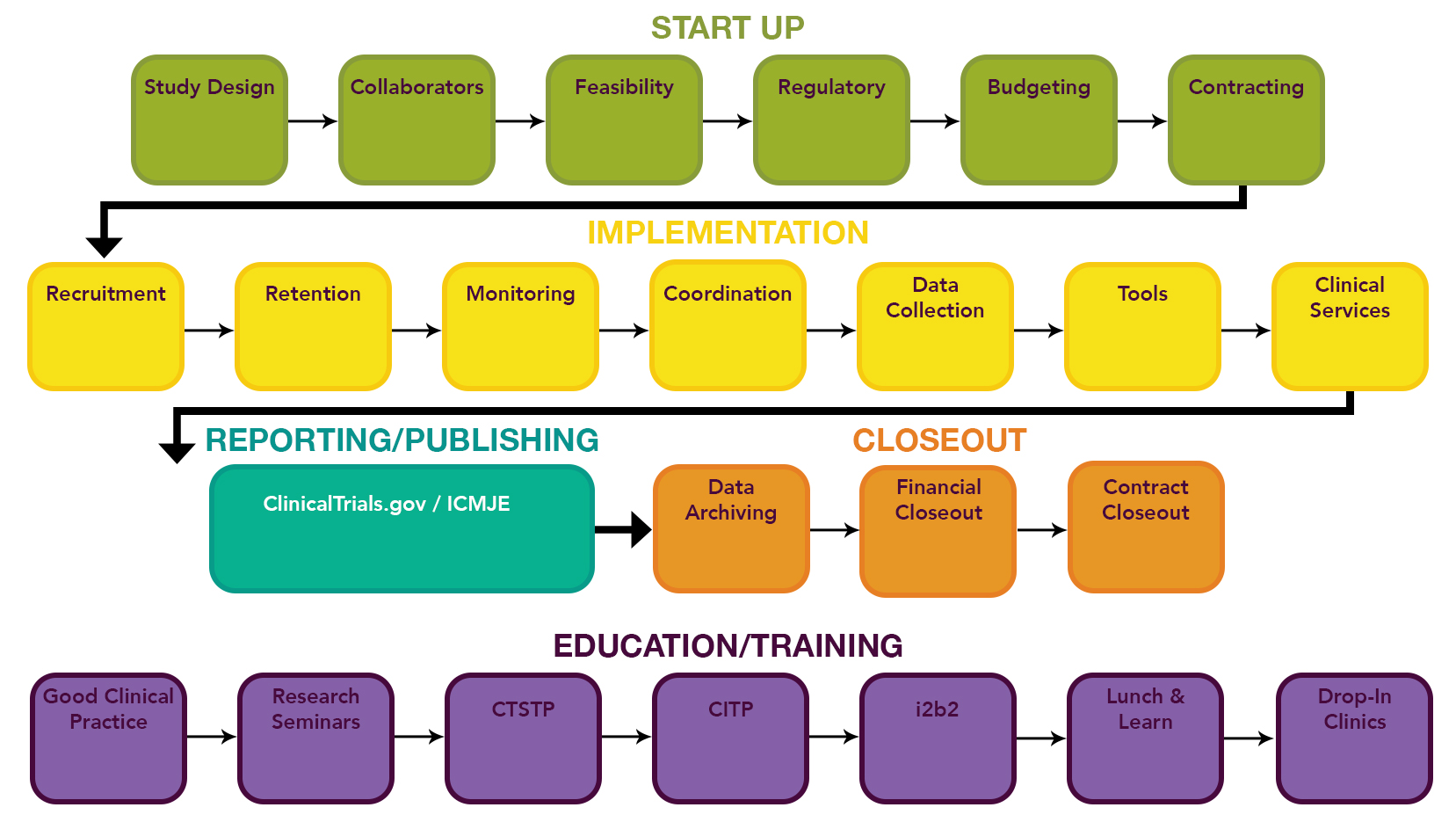
- It can include a Clinical Trial Process Stage, such as:
- Clinical Trial Protocol Design Stage.
- Clinical Trial Site Selection and Activation Stage.
- Clinical Trial Participant Recruitment and Enrollment Stage.
- Clinical Trial Implementation Stage.
- Clinical Trial Intervention and Follow-up Stage.
- Clinical Trial Data Management and Analysis Stage.
- Clinical Trial Closeout Stage.
- Clinical Trial Dissemination of Results Stage.
- Clinical Trials Start-up Stage.
- ...
- It can be associated to a Clinical Trial Participant Journey Model.
- …
- Example(s):
- …
- See: Patient Perspective, Clinical Trial Sponsor Perspective.
References
https://www.appliedclinicaltrialsonline.com/view/ctms-what-you-should-know https://www.clinicaltrialsarena.com/news/operational-excellence-in-clinical-trials-4853862-2/
2023
- chat.openai.com
- Q: What are some of the typical stages in the process of delivering clinical trials?
- A: The process of delivering clinical trials typically involves a number of stages, including:
- Planning and design: This stage involves developing the study protocol, which outlines the details of the study, such as the research question being studied, the study population, the interventions being tested, and the data that will be collected. The protocol must be reviewed and approved by an ethical review board before the study can proceed.
- Site selection and activation: The research team must select the locations where the study will be conducted and ensure that the study sites are ready to begin enrolling and treating patients.
- Participant recruitment and enrollment: The research team will recruit and enroll participants for the study, following the eligibility criteria and informed consent process outlined in the protocol.
- Intervention and follow-up: During this stage, the research team will administer the interventions being tested to the study participants and collect data on their health outcomes. Follow-up visits and assessments will be conducted according to the study protocol.
- Data management and analysis: The research team will organize and analyze the data collected during the study.
- Study closeout: After the study has been completed, the research team will close out the study by completing all final study procedures, such as preparing study reports and submitting the results for publication.
- Dissemination of results: The research team will disseminate the results of the study to the scientific community and the general public through publications in scientific journals and presentations at conferences.
2021
2020
- https://www.uab.edu/ccts/clinical-research/clinical-trials-lifecycle
- QUOTE: ... CCTS supports every stage of the clinical trial lifecycle. ...
- QUOTE: ... CCTS supports every stage of the clinical trial lifecycle. ...
2018
- (Sommer et al., 2018) ⇒ Carsten Sommer, Diego Zuccolin, Valdo Arnera, Nicole Schmitz, Pernilla Adolfsson, Nicoletta Colombo, Raphaelle Gilg, and Bryan McDowell. (2018). “Building Clinical Trials Around Patients: Evaluation and Comparison of Decentralized and Conventional Site Models in Patients with Low Back Pain.” In: Contemporary Clinical Trials Communications, 11. https://doi.org/10.1016/j.conctc.2018.06.008
- QUOTE:

- QUOTE:
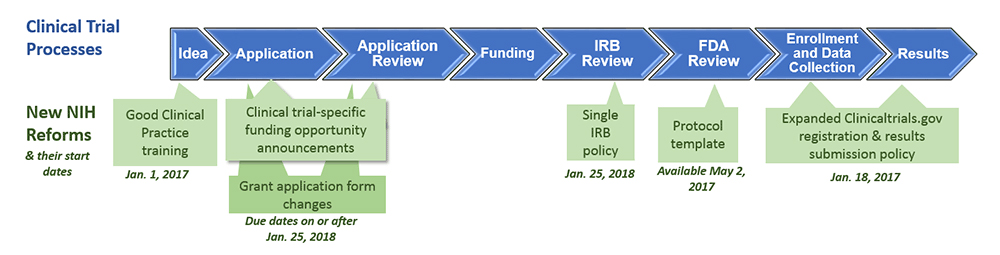
2017
2016
- https://www.nidcd.nih.gov/research/clinical-studies/researchers-professionals/understand-clinical-trials-changes-at-NIH
- QUOTE: For several years, increasing numbers of life sciences organizations have implemented a Clinical Trial Management System (CTMS) that can provide insights gleaned from the system’s data to gain early and increased visibility into problems, progress and possibilities. Many organizations have a constant need to expand CTMS capabilities, integrate clinical operations data across multiple systems, and update clinical trial processes – all in order to adapt to changing regulatory requirements and clinical trial practices. ...

- A life sciences organization exploring the selection of a CTMS should anticipate the solution to provide the following core capabilities:
- Clinical program/project management - Enables oversight of related clinical trials per therapeutic area based on a set of specific clinical project activities (i.e., tracking actual vs. target). Includes the ability to track progress at specific trial and program levels.
- Trial and site planning - Facilitates investigator and site identification and recruitment, including key trial milestone tracking such as target site/enrollment metrics for each study country.
- Site and subject management - Provides tracking ability for site monitoring, subject enrollment relative to plan, and Case Report Form (CRF)/ Electronic Case Report Form (eCRF) completion status. Includes management of site visits/trip reports.
- Study management - Tracks key information such as CRF collection, Clinical Research Associate (CRA) monitoring frequency, protocol visit frequency, and adherence to protocol regiments. Includes support for study documentation and tracking tasks.
- Investigator management - Allows the trial sponsor to manage relationships with investigators, based on visibility into the status study data and related status with CROs and/or investigator sites. Also tracks approvals by Institutional Review Boards (IRB) and Independent Ethics Committees IEC(s).
- Study financials and investigator grants and payment management - Supports financial management including tracking study costs, reimbursing investigators, and paying claims related to study activities. Includes grant payment management and management of financial disclosure.
- Clinical supply management including supply tracking - Manages clinical supplies.
- Clinical trial performance and reporting - Provides reporting/dashboards to communicate trial performance against targets, as well as other operational reports.
- In addition, many current CTMS vendors are offering solutions with advanced capabilities for managing clinical trials that are beyond the scope of traditional CTMS solutions. Among these are:
- Protocol and study documentation management - Enables review/management and authoring of essential study documents. Also includes approval of clinical trial documentation and tracking its status throughout its lifecycle.
- CRF and eCRF development - Provides the ability to view and track the creation of CRF/eCRF forms including their status.
- Tracking electronic data capture (EDC) components and summary details - Tracks the status of data collected in these forms which, in turn, informs the tracking of key clinical trial milestones (e.g., Last Patient Visit (LPV).
- Financial system integration - Integrates SAP financial systems with pre-existing SAP workflows/business rules for payments, including invoicing approvals.
- Clinical supply management: storage and shipment - Extends clinical supply management to include oversight and management of clinical supply logistics for components such as inventory locations, lots, and shipment details.
- Clinical data archiving/warehousing and management - Provides enhanced data management and archiving for future reference
- Data analysis and query resolution - Supports the evaluation of trial-generated clinical data and resolution of any discrepancies or inconsistencies found in clinical data.
- Clinical learning and training - Integrates learning management to track and manage internal and external staff learning requirements relative to the clinical trial process.
- QUOTE: For several years, increasing numbers of life sciences organizations have implemented a Clinical Trial Management System (CTMS) that can provide insights gleaned from the system’s data to gain early and increased visibility into problems, progress and possibilities. Many organizations have a constant need to expand CTMS capabilities, integrate clinical operations data across multiple systems, and update clinical trial processes – all in order to adapt to changing regulatory requirements and clinical trial practices. ...